Testicular varicocele
back to main page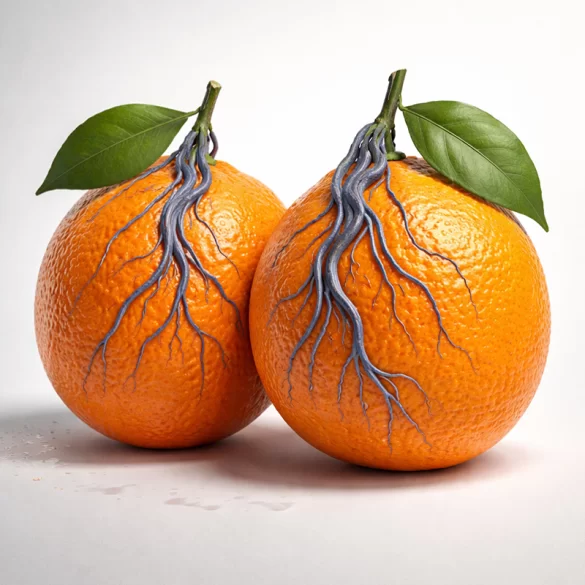

Varicoceles, medically referred to as varicocele of the spermatic cord (varicocele), are pathological dilations and tortuosities of the venous plexus within the scrotum, responsible for draining blood from the testicle. This condition primarily affects young men and is one of the most common causes of reduced male fertility. In many cases, varicoceles are asymptomatic and are detected incidentally during a urological examination or infertility diagnostics. However, in some patients, they lead to pain, a feeling of heaviness in the scrotum, and a progressive deterioration of semen parameters. From a medical standpoint, this issue has significance not only from an aesthetic or comfort perspective but primarily from a functional and hormonal standpoint, as chronic venous outflow disturbances affect testicular temperature, the metabolism of reproductive cells, and testosterone production.
Varicocele – what do they look like
The clinical picture of testicular varicocele is varied and depends on the stage of the disease. In the early stages, changes may be invisible to the naked eye and detectable only through palpation or ultrasound examination using the Valsalva maneuver.
Typical features of the appearance of testicular varicoceles include:
- enlarged, twisted veins within the scrotum, most often on the left side,
- a palpably detectable "bag of worms" sensation,
- asymmetry of the scrotum, with its lower position on the affected side,
- possible reduction in testicular volume (testicular atrophy) in advanced cases.
Subjective symptoms that often accompany anatomical changes include:
- dull, dragging pain that worsens when standing,
- a feeling of heaviness or discomfort in the scrotum,
- worsening of symptoms during physical exertion or prolonged standing,
- reduction of symptoms when lying down.
It is worth emphasizing that the absence of visible changes does not exclude clinically significant varicocele. Many patients experience disturbances in semen parameters despite minimal local symptoms.
Varicocele – types
The classification of testicular varicoceles is based both on the side of occurrence and the degree of clinical advancement.
Classification by location
- Left-sided varicoceles – account for over 80% of cases; they result from the distinct anatomy of venous drainage, where the left testicular vein drains into the renal vein at a right angle.
- Right-sided varicoceles – occur rarely and always require further diagnostics for abdominal or retroperitoneal pathology.
- Bilateral varicoceles – are more common than previously thought, especially in ultrasound examinations.
Clinical classification (grading scale)
- Grade I – varicoceles not palpable, visible only in ultrasound or during the Valsalva maneuver.
- Grade II – varicoceles palpable in an upright position.
- Grade III – varicoceles visible to the naked eye, with noticeable scrotal deformity.
Clinical significance is determined not only by the degree of advancement but also by the impact of changes on:
- semen parameters,
- testicular volume,
- levels of sex hormones,
- the patient's pain discomfort.
Causes of testicular varicose veins
The etiology of varicocele is multifactorial and primarily associated with venous outflow disorders. A key role is played by venous valve insufficiency, leading to blood backflow and increased pressure in the pampiniform plexus.
The most important pathogenic factors include:
- anatomical conditions (especially on the left side),
- congenital weakness of the venous vessel walls,
- venous valve dysfunctions,
- chronic increase in intra-abdominal pressure.
Factors conducive to the development of varicocele:
- intense physical activity with heavy loads,
- prolonged standing work,
- chronic constipation,
- obesity,
- puberty, associated with rapid growth of the testes and blood flow.
From a physiological perspective, the hemodynamic consequences are particularly significant:
- increased testicular temperature,
- tissue hypoxia,
- oxidative stress,
- damage to Sertoli and Leydig cells.
These mechanisms lead to deteriorated spermatogenesis, reduced sperm quality, and hormonal disorders.
Varicocele – treatment
The therapeutic approach for varicocele depends on the patient's age, severity of symptoms, stage of changes, and reproductive plans. Not every case requires surgical treatment.
Recommended for patients:
- without pain symptoms,
- with normal semen parameters,
- without signs of testicular atrophy.
Observation includes regular urological examinations, scrotal ultrasound, and periodic semen analysis.
Surgical and Procedural Treatment
Indications for active treatment:
- pain or discomfort persisting despite conservative treatment,
- abnormal semen parameters,
- testicular atrophy, particularly in young patients,
- male infertility associated with varicocele.
Methods used:
- Microsurgical varicocelectomy – considered the most effective method with the lowest recurrence rate,
- Laparoscopic ligation of testicular veins,
- Endovascular embolization – a minimally invasive method performed by an interventional radiologist.
Treatment effects:
- Improvement in semen parameters (usually after 3–6 months),
- Reduction in pain symptoms,
- Stabilization or improvement in testicular volume,
- Improved fertility in some patients.
It should be clearly stated that treatment of varicocele does not guarantee the restoration of fertility, but in many cases it significantly increases reproductive chances and improves gonadal function.

